In early 2025, the UK government announced plans to abolish NHS England – the independent body responsible for overseeing the NHS. The objective is to bring the health service under direct government control, cut bureaucracy, and improve ministerial accountability. While some view this as a bold step toward efficiency, others believe the planned NHS reform could increase political interference, disrupt services, and lead to job losses within the system.
As the UK government moves forward with these proposed reforms to the NHS, Pureprofile conducted a nationally representative survey of 501 Brits, to explore public opinion on NHS reform, how the public perceive the potential implications for how the NHS operates, its overall efficiency, and the future of healthcare in the UK.
A complex mix of optimism and concern
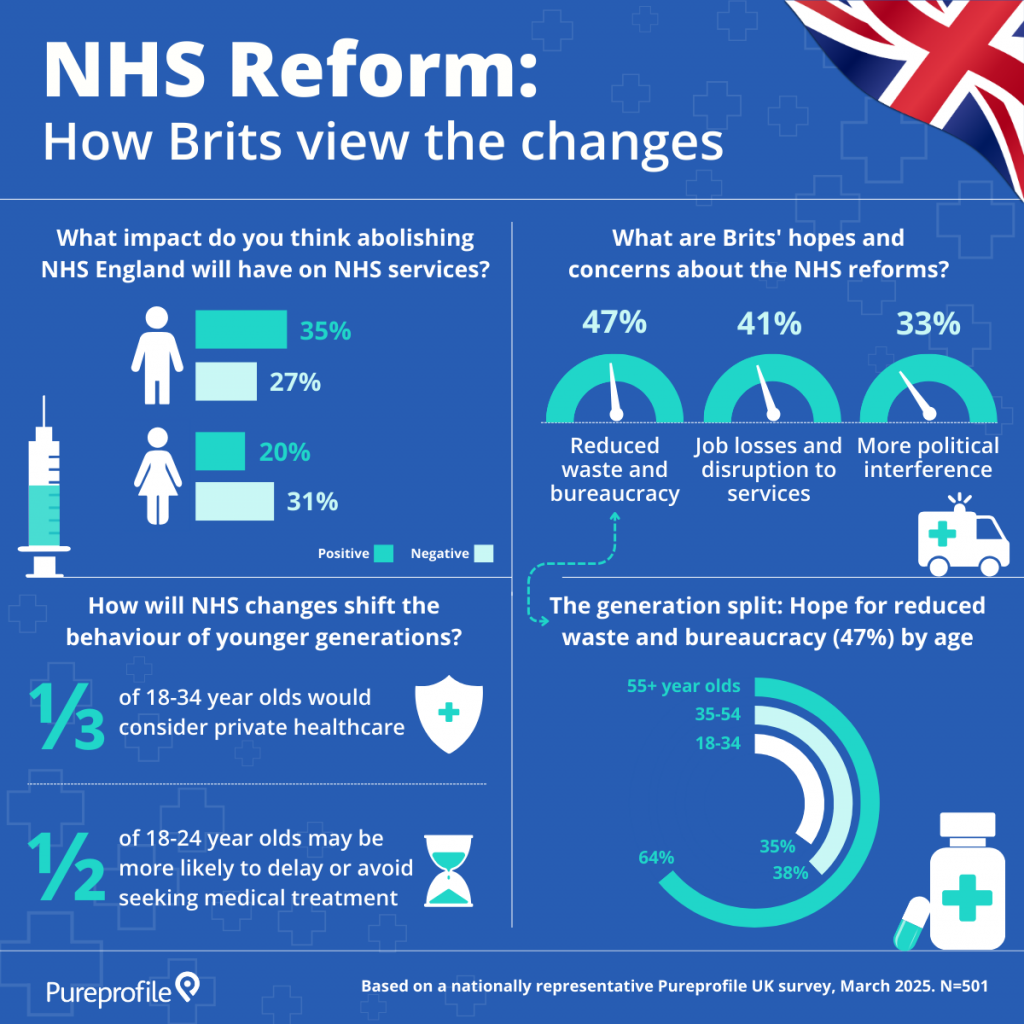
Public reaction to the proposed NHS reforms reveals a nuanced picture, with people weighing potential benefits against perceived risks. A clear gender divide highlights how the changes are being interpreted differently across the population. When asked how they believe the reforms will affect NHS service.
35% of men think the NHS reforms will have a positive impact
31% of women think the NHS reforms will have a negative impact
Looking more broadly at public sentiment, the hopes and concerns reflect a split between optimism and unease:
47% of Brits are hopeful that the reforms could reduce waste and bureaucracy
41% are concerned about job losses and disruption to services
33% are concerned about more political interference in the NHS
The findings indicate that while the promise of streamlining the NHS is resonating with many Brits, a significant portion of the population remains wary of unintended consequences, particularly around potential disruption, job security, and the increased role of government in managing NHS operations.
Older Brits are more optimistic about efficiency
A closer look at the 47% of Brits who are hopeful the reforms will reduce waste and bureaucracy, reveals that this view is not evenly shared across age groups.
64% of those aged 55+ believe the changes could help reduce waste and bureaucracy, while only 38% of 35–54 year olds and 35% of 18–34 year olds feel the same
This generational split may reflect differing levels of experience to how the NHS has evolved over time. Older adults, with more lived experience with NHS systems and witnessing changes first-hand, may feel more confident that reform could bring long-overdue improvements in efficiency.
By contrast, younger adults may have grown up in a context of increasing strain on the NHS which could explain a more sceptical view of the proposed changes to the UK healthcare system.
Younger generations are rethinking healthcare choices
While much of the national conversation around reform focuses on opinions and expectations, the findings indicate that some younger people are re-evaluating how they might access healthcare in light of the proposed NHS changes.
1 in 3 people aged 18–34 say they would consider private healthcare
1 in 2 aged 18–24 may be more likely to delay or avoid seeking medical treatment altogether
This potential shift in mindset raises important questions about the long-term engagement of younger adult populations with public services, and what that could mean for access and care in the years ahead.
Our survey findings highlight public reaction to the proposed NHS reform is far from unanimous. As the conversation continues, policymakers will need to navigate not only the operational challenges of the restructure, but also the diverse expectations, hopes, and growing concerns held by the public.
The infographic below represents key findings from our research: